Abstract
Background Olverembatinib is a novel third-generation BCR-ABL1 tyrosine kinase inhibitor (TKI) with antitumor activity against CML and Ph+ ALL regardless of genotype and a preliminarily favorable human safety profile. This study is the first to report on the safety, efficacy, and pharmacokinetic (PK) profiles of olverembatinib in patients with CML (all phases) and Ph+ ALL outside China, whose disease failed ponatinib treatment and at least 2 prior TKI treatments.
Methods In this multicenter, open-label, randomized trial, olverembatinib is administered orally on alternate days (QOD) in adults with chronic-phase (CP-CML), accelerated-phase (AP-CML), or blast-phase CML (BP-CML) or Ph+ ALL. Enrolled patients have had no fewer than 2 prior TKI failures, except for those whose disease harbors T315I mutation, for whom the number of previous TKIs is not limited. Study participants are randomized 3:3:2 to olverembatinib 30, 40, or 50 mg QOD in 28-day cycles.
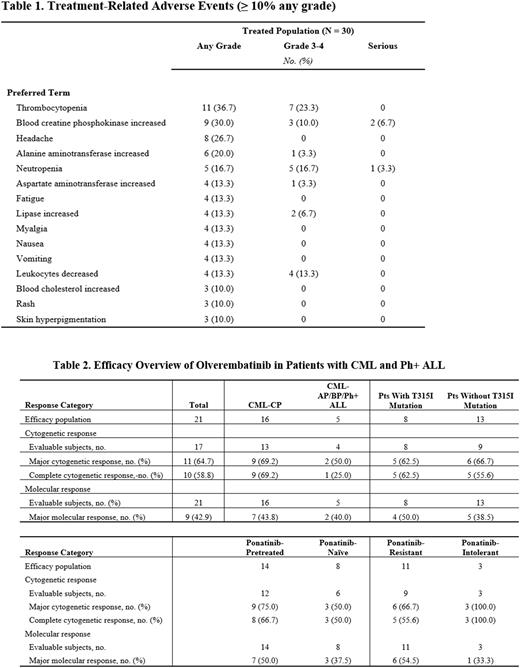
Results A total of 30 patients have been enrolled, including 23 with CP-CML, 4 with AP-CML, 2 with BP-CML, and 1 with Ph+ ALL. The median (range) treatment duration is 4.8 (0.03-21.29) months and the median (range) interval from CML/Ph+ ALL diagnosis to olverembatinib treatment onset, 7.0 (1.5-24.0) years. Half (15/30) of patients are men, and the median (range) age is 47.0 (21.0-74.0) years. In all, 1 (3.3%), 7 (23.3%), 8 (26.7%), and 9 (30.0%) patients received 2, 3, 4, and ≥ 5 prior TKIs, respectively. A total of 21 (70.0%) patients were pretreated with third-generation TKI ponatinib, including 17 (81.0%) with resistance and 4 (19.0%) with intolerance; a total of 5 (16.7%) were pretreated with asciminib; 12 (40.0%) had T315I mutations; and 13 (43.3%), hypertension. At baseline, all patient BCR-ABL1IS levels were > 1%. Olverembatinib was well tolerated. Twenty-two (73.3%) patients experienced any-grade treatment-related AEs (TRAEs; Table 1), incidences of which tended to be dose-dependent. Most nonhematologic TRAEs were grade 1/2. Common grade 3/4 hematologic TRAEs included thrombocytopenia (7/30; 23.3%), neutropenia (5/30; 16.7%), and decreased leukocyte counts (4/30; 13.3%). In all, 11 (36.7%) of 30 patients experienced serious AEs, of which 6 (20.0%) were considered olverembatinib-related and 1 (3.3%) led to treatment discontinuation. One patient with AP-CML from the 50-mg dose cohort died of progressive disease. Olverembatinib conferred potent antileukemic activity in patients with CML and Ph+ ALL (Table 2). Of 21 efficacy-evaluable patients, 17 were evaluable for cytogenetic response, of whom 10 (58.8%) had complete cytogenetic response (CCyR); 9/21 (42.9%) patients had major molecular responses (MMR). Olverembatinib was effective in patients with either T315I-mutant (62.5%, CCyR; 50%, MMR) or T315IWT (55.6%, CCyR; 38.5%, MMR), and its effectiveness was not compromised by prior use of ponatinib or asciminib. Among patients pretreated with ponatinib with available responses, 5 (55.6%) of 9 patients with ponatinib-resistant disease experienced CCyR and 6 (54.5%) of 11, MMR. Four of 5 patients pretreated with asciminib showed response. PK analyses indicated an approximately dose-proportional increase in olverembatinib plasma exposure from 30 to 50 mg QOD and comparable plasma exposure between Chinese and US CML populations.
Conclusions Olverembatinib monotherapy is efficacious and well tolerated in patients with TKI-refractory CML and Ph+ ALL. Even in patients with CML who were ponatinib or asciminib resistant, or who had T315I mutations, olverembatinib showed strong efficacy. This analysis confirms that olverembatinib is a potentially viable treatment option for patients with CML and Ph+ ALL, including those with ponatinib failure or T315I mutation. Internal study identifier: HQP1351-CU101. Clinicaltrials.gov identifier: NCT04260022.
Disclosures
Jabbour:Amgen: Other: Advisory Role, Research Funding; Genentech: Other: Advisory Role, Research Funding; Bristol Myers Squibb: Other: Advisory Role, Research Funding; Spectrum: Research Funding; Adaptive Biotechnologies: Other: Advisory Role, Research Funding; Pfizer: Other: Advisory Role, Research Funding; Takeda: Other: Advisory Role, Research Funding; AbbVie: Other: Advisory Role, Research Funding. Koller:Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Speakers Bureau; Takeda: Speakers Bureau; Treadwell Therapeutics: Other: Safety Review Committee. Oehler:Pfizer: Consultancy, Research Funding; Novartis: Consultancy; Blueprint Medicines: Consultancy; Bristol Myers Squibb: Consultancy. Mukherjee:BMS: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Advisor or review panel participant, Research Funding; Eusa Pharma: Consultancy, Other: Advisor or review panel participant; Teaching and Speaking; Genentech: Membership on an entity's Board of Directors or advisory committees; Blueprint Medicines: Membership on an entity's Board of Directors or advisory committees, Other: Advisor or review panel participant; Partnership for Health Analytic Research, LLC: Honoraria; Novartis: Consultancy, Membership on an entity's Board of Directors or advisory committees, Other: Advisor or review panel participant, Research Funding; BioPharm: Consultancy; Jazz Pharmaceuticals: Other: Principal investigator for Investigator Initiated Trials (the Institution gets the funding), Research Funding; Celgene/Acceleron: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Other: Advisor or review panel participant, Research Funding; AbbVie: Membership on an entity's Board of Directors or advisory committees, Other: Advisor or review panel participant; Aplastic Anemia and MDS International Foundation: Honoraria; McGraw Hill Hematology Oncology Board Review: Honoraria, Other: Advisor or review panel participant. Baer:Kura Oncology: Research Funding; AbbVie: Research Funding; Forma: Research Funding; Kite, a Gilead Company: Research Funding; Takeda: Research Funding; Ascentage: Research Funding. Beck:Highlands Oncology Group: Research Funding. Chen:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company. Guo:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company. Fu:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company. Men:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company. Wang:Ascentage Pharma: Current Employment. Yang:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company, Other: Leadership, Patents & Royalties. Zhai:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company, Other: Leadership, Patents & Royalties. Kantarjian:Ipsen Pharmaceuticals: Honoraria, Membership on an entity's Board of Directors or advisory committees; Astellas Health: Honoraria, Membership on an entity's Board of Directors or advisory committees; AbbVie: Honoraria, Research Funding; Amgen: Honoraria, Research Funding; Ascentage: Membership on an entity's Board of Directors or advisory committees, Research Funding; Novartis: Honoraria, Research Funding; Pfizer: Honoraria, Research Funding; NOVA Research: Honoraria; KAHR Medical Ltd: Honoraria, Membership on an entity's Board of Directors or advisory committees; ImmunoGen: Research Funding; Daiichi-Sankyo: Consultancy, Research Funding; Jazz Pharmaceuticals: Research Funding; Takeda: Honoraria. Jiang:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company. Wang:Ascentage Pharma: Current Employment, Current equity holder in publicly-traded company.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal